Lumbosacral Disc Disease ICD 10: A Deep Dive Into Understanding And Managing This Condition
Alright, listen up, folks. Today we’re diving deep into a topic that affects millions worldwide but often gets overlooked: lumbosacral disc disease ICD 10. If you’ve ever felt that nagging pain in your lower back or experienced numbness shooting down your legs, this might just be the article you need. We’re not here to scare you; instead, we’re here to break it down in a way that makes sense—because knowledge is power, right?
Now, before we dive into the nitty-gritty, let’s talk about why this matters. Lumbosacral disc disease isn’t just some fancy medical term; it’s a real condition that impacts daily life. Whether you’re an athlete, a desk jockey, or someone who spends hours on their feet, understanding this condition can help you take control of your health. Stick around, because we’re about to uncover everything you need to know.
Here’s the deal: this article isn’t just another boring medical explanation. We’re going to make this journey as engaging as possible, breaking down complex terms into bite-sized pieces. By the end of this, you’ll not only understand what lumbosacral disc disease is but also how to manage it effectively. So, let’s get started!
- Tyson Career Record A Knockout Journey Through Boxing History
- How To Decode Your Ez Pass Transponder Number Like A Pro
What Exactly is Lumbosacral Disc Disease?
Let’s start with the basics. Lumbosacral disc disease refers to a condition where the discs located between the vertebrae in your lower back (lumbar and sacral regions) start to degenerate or herniate. Think of these discs as cushions that absorb shock and allow smooth movement. When they’re damaged, it can lead to a whole host of problems, from back pain to sciatica.
Here’s the kicker: this condition is more common than you think. According to recent studies, nearly 80% of adults will experience lower back pain at some point in their lives. While not all cases are severe, understanding the symptoms and treatment options can make all the difference.
Key Symptoms to Watch Out For
Now, let’s talk symptoms. The earlier you catch these signs, the better your chances of managing the condition. Here’s a quick rundown:
- How Many Seasons Are There Of Heartland A Deep Dive Into The Heartwarming Series
- Astrology Chart Rising Sign Unveiling The Mysteries Of Your True Self
- Persistent lower back pain that worsens with movement
- Numbness or tingling in the legs
- Weakness in the muscles of the legs or feet
- Difficulty standing or walking for extended periods
- Pain that radiates down the buttocks and legs (sciatica)
Remember, these symptoms can vary from person to person. Some might experience mild discomfort, while others could be dealing with debilitating pain. If any of these sound familiar, it’s time to consult a healthcare professional.
ICD-10 Codes: Why They Matter
Alright, let’s talk about the elephant in the room: ICD-10 codes. For those who aren’t familiar, ICD-10 stands for International Classification of Diseases, Tenth Revision. These codes are used by healthcare providers to classify and report medical diagnoses. Why does this matter? Because accurate coding ensures proper diagnosis, treatment, and billing.
For lumbosacral disc disease, the relevant ICD-10 codes include:
- M51.0 – Herniated disc, lumbar region
- M51.2 – Other intervertebral disc displacement, lumbar region
- M50.3 – Cervical disc disorder with radiculopathy
These codes might seem like a bunch of random letters and numbers, but they play a crucial role in your healthcare journey. Make sure to double-check with your doctor to ensure the correct code is being used for your condition.
How Are ICD-10 Codes Used in Treatment?
Here’s the deal: ICD-10 codes aren’t just for billing purposes. They also guide treatment plans. For example, if your doctor codes your condition as M51.0 (herniated disc), it might lead to a different treatment approach compared to M51.2 (displacement). This is why accuracy is key.
Pro tip: Always ask for a copy of your medical records to ensure everything is documented correctly. It’s your health, after all!
Causes and Risk Factors
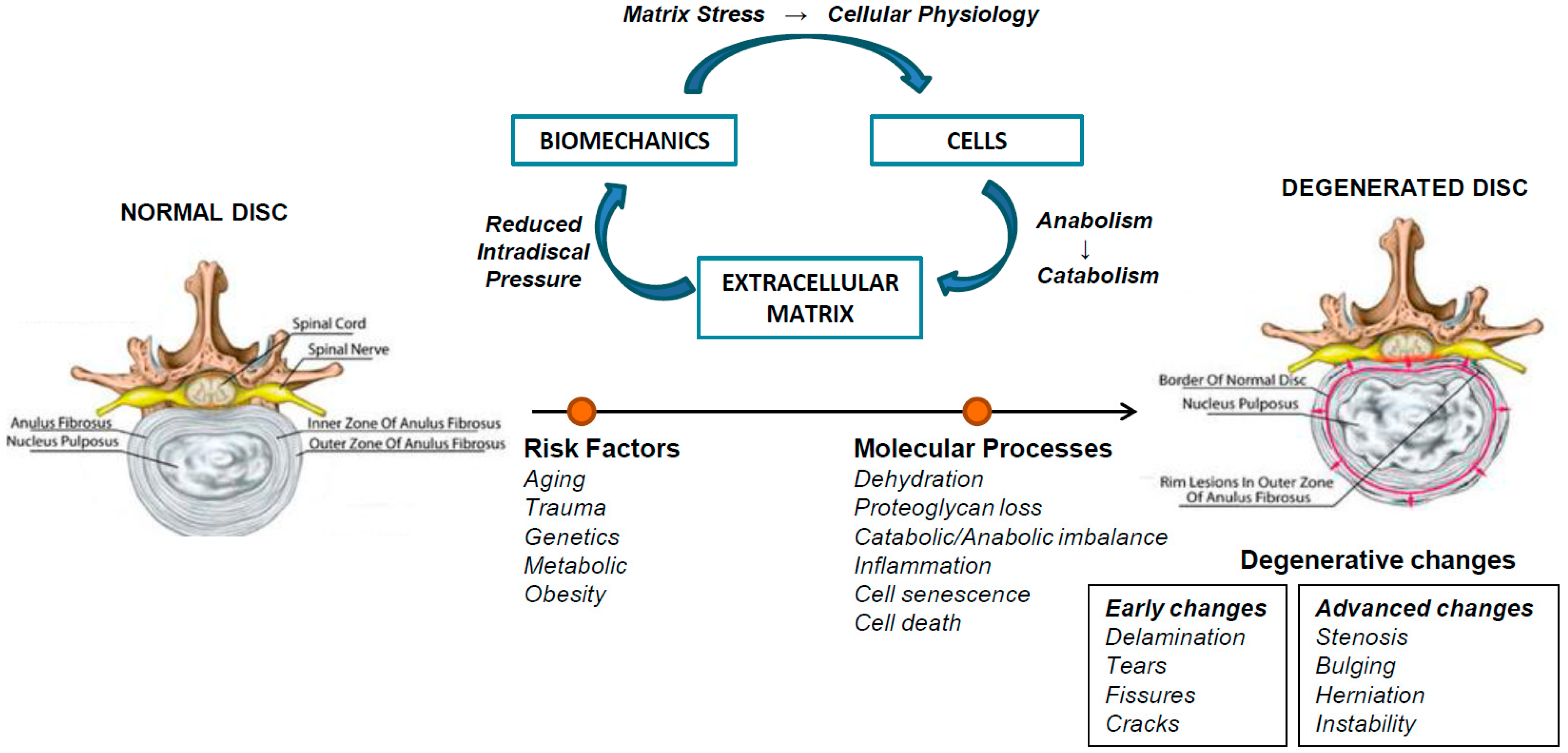
So, what causes lumbosacral disc disease? Let’s break it down. The most common causes include:
- Aging and natural wear and tear of the discs
- Injury or trauma to the lower back
- Repetitive strain from activities like heavy lifting or poor posture
- Genetic factors that predispose some individuals to disc degeneration
Risk factors can vary, but here are a few to keep in mind:
- Age: The older you get, the higher your risk
- Obesity: Excess weight puts additional strain on your spine
- Sedentary lifestyle: Lack of exercise weakens the muscles supporting your back
Now, here’s the good news: many of these risk factors are modifiable. With the right lifestyle changes, you can significantly reduce your chances of developing this condition.
Prevention Strategies
Let’s talk prevention. While we can’t stop the aging process, we can take steps to protect our spines. Here’s what you can do:
- Maintain a healthy weight
- Engage in regular physical activity, focusing on core strengthening exercises
- Practice good posture, especially if you have a desk job
- Avoid heavy lifting or use proper techniques when lifting
Small changes can make a big difference. Trust me, your back will thank you later!
Diagnosis: How Do Doctors Detect Lumbosacral Disc Disease?
Alright, let’s talk diagnosis. If you suspect you have lumbosacral disc disease, your doctor will likely perform a series of tests to confirm. These may include:
- Physical examination to assess range of motion and identify areas of pain
- Imaging tests like X-rays, MRIs, or CT scans to visualize the discs and surrounding structures
- Nerve conduction studies to evaluate nerve function
Each test provides valuable information, helping your doctor piece together the puzzle. Remember, early detection is key to effective treatment.
Why Early Diagnosis Matters
Here’s the thing: the sooner you catch lumbosacral disc disease, the better your chances of managing it without invasive procedures. Early diagnosis allows for conservative treatments like physical therapy and medication, which can often provide relief without surgery.
So, if you’re experiencing symptoms, don’t hesitate to seek medical attention. Your back will thank you!
Treatment Options: What Works Best?
Now, let’s talk treatment. The approach depends on the severity of your condition, but here’s a general breakdown:
Non-Surgical Treatments
- Physical therapy: Exercises to strengthen the core and improve flexibility
- Medications: Pain relievers, anti-inflammatory drugs, or muscle relaxants
- Epidural steroid injections: To reduce inflammation around the nerves
Surgical Interventions
In severe cases, surgery might be necessary. Common procedures include:
- Discectomy: Removal of part of the damaged disc
- Spinal fusion: Joining vertebrae to stabilize the spine
- Artificial disc replacement: Replacing the damaged disc with an artificial one
While surgery might sound daunting, advancements in technology have made these procedures safer and more effective than ever before.
Lifestyle Changes: The Key to Long-Term Relief
Let’s talk about the elephant in the room: lifestyle changes. Whether you’re undergoing treatment or trying to prevent the condition, making small adjustments can make a big difference. Here’s what you can do:
- Stay active: Regular exercise keeps your muscles strong and flexible
- Practice mindfulness: Techniques like yoga and meditation can reduce stress and improve posture
- Invest in ergonomic furniture: A supportive chair and desk setup can prevent strain
Remember, consistency is key. It’s not about doing everything perfectly; it’s about making gradual improvements over time.
Staying Positive: The Power of Mindset
Here’s the thing: living with chronic pain can be tough, but your mindset plays a huge role in how you cope. Surround yourself with supportive people, and don’t hesitate to seek professional help if needed. You’ve got this!
Resources and Support
Finally, let’s talk resources. If you’re dealing with lumbosacral disc disease, you’re not alone. There are countless organizations and communities dedicated to supporting individuals with spinal conditions. Here are a few to check out:
- North American Spine Society
- Spine-health
- Arthritis Foundation
These resources offer everything from educational materials to support groups, helping you navigate your journey with confidence.
Final Thoughts
Alright, folks, that’s a wrap. We’ve covered a lot today, from understanding lumbosacral disc disease ICD 10 to exploring treatment options and lifestyle changes. Remember, knowledge is power, and taking control of your health is the first step toward recovery.
So, what’s next? Leave a comment below and let us know your thoughts. Have you dealt with this condition? What worked for you? And don’t forget to share this article with someone who might benefit from it. Together, we can spread awareness and make a difference!
Disclaimer: This article is for informational purposes only and should not replace professional medical advice. Always consult your healthcare provider for personalized guidance.
Table of Contents
- What Exactly is Lumbosacral Disc Disease?
- ICD-10 Codes: Why They Matter
- Causes and Risk Factors
- Diagnosis: How Do Doctors Detect Lumbosacral Disc Disease?
- Treatment Options: What Works Best?
- Lifestyle Changes: The Key to Long-Term Relief
- Resources and Support
- Pain In Stomach From Coughing Why It Happens And How To Fix It
- Ronnie Mcnutt The Life Legacy And Impact Of A Forgotten Icon
Degenerative Disc Disease Lumbar Icd 10 Quotes Trendy

Degenerative Disc Disease Progression, Symptoms, and Chiropractic

Phases Of Degenerative Disc Disease